Recurrent yeast infections, medically known as recurrent vulvovaginal candidiasis (RVVC), can be an incredibly frustrating and uncomfortable experience for many women. Characterized by the frequent recurrence of symptoms like itching, burning, and vaginal discharge, RVVC can significantly impact a person’s quality of life. In this blog post, we will delve into the underlying causes of recurrent yeast infections, explore the factors that contribute to the vicious cycle, and discuss some of the breakthrough treatments that offer hope for those seeking relief.
The Basics Of Yeast Infections
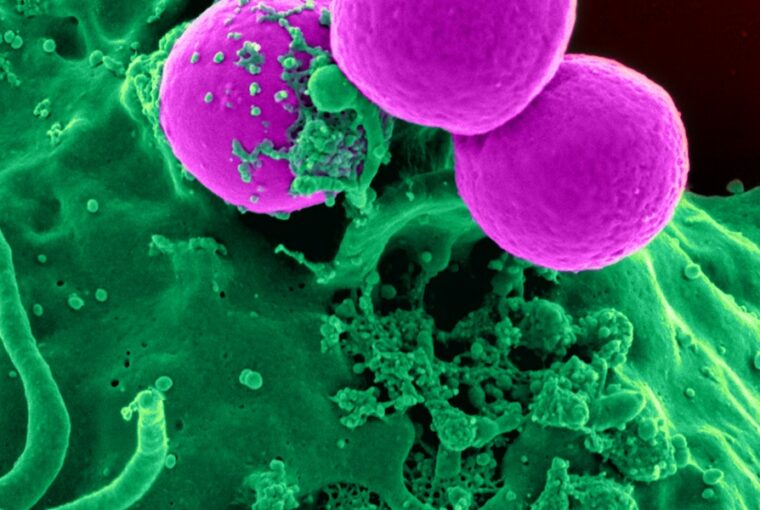
Yeast infections are primarily caused by an overgrowth of the fungus Candida, most commonly Candida albicans, in the vaginal area. Candida naturally resides in the vagina, but various factors can disrupt the balance of microorganisms, leading to an overgrowth. These factors include hormonal fluctuations, antibiotic use, weakened immune system, uncontrolled diabetes, and even lifestyle choices like wearing tight synthetic clothing or using scented hygiene products.
The Vicious Cycle Of Recurrent Yeast Infections
For some individuals, a yeast infection is not a one-time occurrence but rather a recurring issue. This cycle of recurrence can be frustrating and perplexing. One yeast infection is treated, only for another to appear shortly after. This cycle may be perpetuated by several factors:
Incomplete Treatment
Sometimes, yeast infections are treated with over-the-counter antifungal creams or prescription medications, but the treatment is not followed through completely. This can allow some Candida cells to survive and multiply, leading to a relapse.
Resistance
Over time, some strains of Candida can become resistant to commonly used antifungal medications, making them less effective in treating the infection.
Underlying Conditions: Certain underlying health conditions, such as hormonal imbalances, diabetes, or immune system disorders, can make individuals more susceptible to recurrent yeast infections.
Disruption of the Microbiome
An imbalance in the vaginal microbiome, which includes various types of bacteria, can create an environment conducive to yeast overgrowth.
Breakthrough Treatments For Recurrent Yeast Infections
Fortunately, medical research has paved the way for breakthrough treatments that offer hope for individuals trapped in the cycle of recurrent yeast infections. These treatments aim to address the root causes of the issue and provide more effective and long-lasting relief. Shop now for treatments.
Boric Acid Suppositories
Boric acid suppositories have gained popularity as an alternative treatment for recurrent yeast infections. Boric acid has antifungal properties and can help restore the vaginal pH balance, creating an environment less favorable for Candida overgrowth.
Lifestyle Modifications
Making certain lifestyle changes can significantly reduce the risk of recurrent yeast infections. This includes wearing breathable cotton underwear, avoiding scented hygiene products, and practicing good hygiene habits.
Probiotics
Probiotics containing specific strains of beneficial bacteria, such as Lactobacillus acidophilus, can help restore the natural balance of the vaginal microbiome, creating an environment less conducive to yeast overgrowth.
Prescription Medications
In cases where antifungal resistance is a concern, healthcare providers may prescribe different classes of antifungal medications or combination therapies for more effective treatment.
Identifying Underlying Conditions
Comprehensive medical evaluation and testing can help identify and address underlying health conditions that contribute to recurrent yeast infections.
Personalized Treatment Plans
Working closely with a healthcare provider to develop a personalized treatment plan based on the individual’s medical history, lifestyle, and specific needs can lead to more successful outcomes.
Prevention Strategies
While addressing recurrent yeast infections is crucial, preventing their occurrence in the first place is equally important. Implementing proactive strategies can significantly reduce the likelihood of falling into the vicious cycle. Here are some key prevention tips:
Maintain Proper Hygiene
Practicing good vaginal hygiene is essential. Opt for mild, unscented soaps and avoid douching, as it can disrupt the vaginal pH balance and lead to yeast overgrowth.
Dietary Adjustments
Some evidence suggests that a diet high in sugar and refined carbohydrates can contribute to yeast overgrowth. Incorporating more probiotic-rich foods like yogurt and fermented vegetables may promote a healthier vaginal microbiome.
Cotton Underwear
Choose breathable, cotton underwear over synthetic fabrics. Cotton helps keep the genital area dry and discourages the growth of Candida.
Avoid Irritants
Steer clear of scented tampons, pads, and feminine hygiene products, as these can irritate the vaginal area and disrupt the natural balance of microorganisms.
Manage Underlying Conditions
If you have underlying health conditions like diabetes, work closely with your healthcare provider to manage them effectively. Well-controlled diabetes can help prevent recurrent yeast infections.
When To Consult A Healthcare Provider
While home remedies and over-the-counter treatments can be helpful, recurrent yeast infections may require professional intervention. Here’s when it’s time to seek the guidance of a healthcare provider:
Frequency of Infections
If you experience more than four yeast infections in a year, it’s important to consult a healthcare provider. Frequent recurrences could indicate an underlying issue that needs to be addressed.
Persistent Symptoms
If your symptoms don’t improve after a few days of treatment or recur shortly after treatment, it’s a sign that a more comprehensive approach is needed.
Severe Discomfort
If your symptoms are particularly severe, causing intense itching, burning, or pain, a healthcare provider can help provide relief and prevent complications.
Unusual Discharge
If you notice unusual vaginal discharge that is greenish, yellowish, or foul-smelling, it’s important to seek medical attention, as this could indicate a different type of infection.
Pregnancy
Pregnant individuals should consult a healthcare provider before using any treatments, as some medications may not be safe during pregnancy.
Taking Charge Of Your Vaginal Health
Recurrent yeast infections can be a frustrating challenge, but armed with knowledge and guidance, you can regain control of your vaginal health. Remember that every individual’s body is unique, and what works for one person may not work for another. By adopting a holistic approach that addresses lifestyle factors, promotes vaginal health, and seeks professional help when needed, you can break free from the vicious cycle of recurrent yeast infections and enjoy greater comfort and well-being.
Conclusion
Recurrent yeast infections can disrupt daily life and lead to discomfort and frustration. However, armed with information about the causes, contributing factors, and available treatments, individuals can take proactive steps to break free from this cycle. By understanding the role of Candida overgrowth, embracing preventive measures, seeking professional guidance, and making informed choices about treatment options, you can regain control over your vaginal health. Remember, you don’t have to navigate this journey alone – healthcare providers are there to support and guide you towards effective solutions. With the right approach and a commitment to your well-being, you can overcome recurrent yeast infections and enjoy a more comfortable and balanced vaginal environment.