Utilizing mouse models, specialists from the University of California Los Angeles have built up a test treatment that lifts the degrees of a sort of insusceptible cell that seems fit for battling a few types of malignancy.
Mouse models like m38 are essential tools for studying human diseases and testing new treatments. By recreating the conditions of a disease in a mouse, researchers can gain valuable insights into the causes and progression of the disease. Mouse models also allow scientists to test the safety and effectiveness of new drugs and therapies before they are used in humans. In some cases, mouse models can even be used to predict how a disease will affect different people based on the genetic differences between mice and humans. As a result, mouse models play an essential role in medical research and provide an invaluable resource for developing new treatments for human diseases.
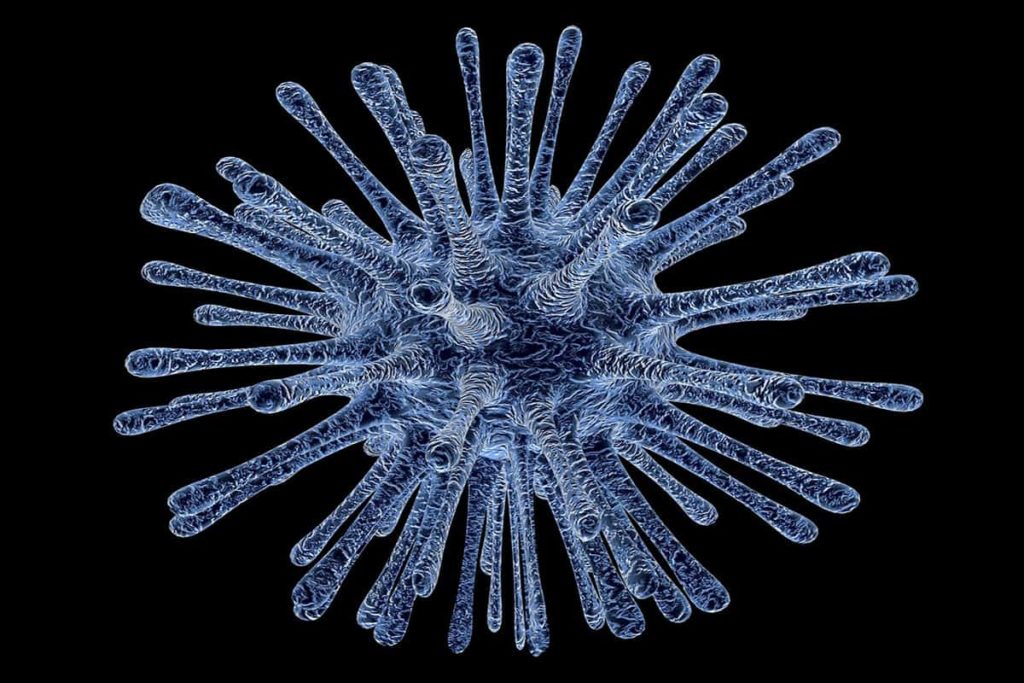
Invariant characteristic executioner T (iNKT) cells are a sort of amazing resistant cell fit for battling a wide range of “interlopers,” including malignant growth cells.
Human bodies hold generally few of these cells, restricting the amount they can add to stifling tumor development. Be that as it may, their strength makes them perfect contender for imaginative anticancer immunotherapy.
What’s more, this is decisively what a group of specialists from the University of California Los Angeles (UCLA) has decided to do. Utilizing mouse models of various types of malignant growth, the researchers have tried another treatment that lifts the capability of iNKT cells.
The scientists detail their investigations in an examination paper that currently shows up in the diary Cell Stem Cell.
In the examination paper, the analysts clarify that what makes these insusceptible cells uncommon is that — in contrast to other safe cells — they “have the wonderful ability to focus on different kinds of malignant growth” on the double.
By taking a gander at past clinical examinations, the scientists likewise found that individuals with malignant growth who normally have more significant levels of iNKT cells will in general live for longer than friends with lower levels.
They are ground-breaking cells, however they’re normally present in such little numbers in the human blood that they as a rule can’t have a remedial effect, Yang clarifies.
Through their ongoing trials, the specialists needed to make a type of treatment that would invigorate the body to create more iNKT cells consistently. The group was wanting to locate a “solitary conveyance” treatment, as it were.
At that point, to check whether the cells filled in as they proposed, the specialists tried HSC-iNKT cells in mice to which they had moved both human bone marrow and malignant growths of human root, including different myeloma (a type of blood disease), and melanoma.
The group found that the test was fruitful: the HSC-iNKT cells had the option to separate and shape iNKT cells, and this procedure proceeded for the remainder of the rodents’ lives. That as well as the mice they had treated likewise introduced powerful concealment of both various myeloma and melanoma tumor development.
One preferred position of this methodology is that it’s a one time cell treatment that can furnish patients with a long lasting stockpile of iNKT cells, says Yang.
The scientists additionally indicate that iNKT cells represented 60% of the all out T cell include in the mice that had the HSC-iNKT treatment in contrast with the control mice, which speaks to a noteworthy lift.
In spite of the fact that this treatment is, so far, just at the degree of preclinical research, and it stays indistinct whether this equivalent procedure would be as powerful in people, the UCLA specialists accept that the reason is promising.